Peter Piot was a young researcher training in virology at the Institute of Tropical Medicine Antwerp in 1976 when some unusual samples from Central Africa arrived at the Belgian lab. They had been taken from a Catholic missionary who had died from an unknown disease in a remote village in the Democratic Republic of the Congo, then known as Zaire.
Piot’s team isolated the virus and christened it “Ebola”, after a river that flowed close to the village. But Piot’s involvement did not end there: he was also keen to fly out to the Congo to help with the relief effort. “I was particularly interested in how this virus was transmitted and what this epidemic is about,” he tells Times Higher Education. “I had never been to Africa and I had no experience investigating epidemics, but there were not that many volunteers…I was 27; it was very exciting.”
By the time Piot and the other 25 or so volunteers arrived, armed with just paper masks, latex gloves and motorbike goggles to protect themselves, the local people were already taking measures to contain the disease, having developed containment techniques after previous smallpox outbreaks. Most of the infected people died but the containment team managed to limit the death toll to about 300. For Piot, it was a “life-changing” experience.
Over the following decades, researchers learned more about the Ebola virus, identifying its five known strains and discovering how it is transmitted between humans through bodily fluids. However, no treatment was developed. Responding to modest outbreaks in Central Africa, the relief agency Médecins Sans Frontières focused on containment and supportive therapy.
Then came the West African outbreak. It began in December 2013 with the death of Emile Ouanmouno, a two-year-old from a remote village in Guinea – followed closely by that of his sister, mother and grandmother. By March 2014, Guinea’s ministry of health was reporting outbreaks of Ebola and cases were appearing in neighbouring Liberia and Sierra Leone. MSF established its first treatment unit in the Guinean town of Guéckédou, and began to warn of an “epidemic of a magnitude never seen before”.
Unlike previous Ebola outbreaks, which were confined to rural communities, the virus struck cities, including the capitals of the three affected countries. Attempts were made to contain it, with whole villages placed under quarantine and traditional burial rituals – which involve contact with the corpse – dispensed with. Yet still the epidemic spread.
“We didn’t expect a big Ebola outbreak like this,” says Adrian Hill, director of the Jenner Institute, the centre for vaccine research at the University of Oxford. “A large one had never happened before, and [never in] West Africa…We were not prepared.”
Since his early work in the Congo, Piot had gone on to earn an international reputation in microbiology. While his more recent work had focused on HIV, he had continued to keep an interested eye on subsequent outbreaks of Ebola and haemorrhagic fever.
“In June [2014], I remember MSF saying that this epidemic was out of control,” he recalls. “I went to Amsterdam, where they had a meeting, and I heard stories from people who had come back [from West Africa]. And I said: ‘This [outbreak] is different.’ And so I went to CNN, I gave an interview…in early July and I called for a state of emergency [to be declared]. I thought after the interview: ‘I am Flemish. We are understated...Why did I say that?’.” The answer, he says, is that “I know that when you have one case of Ebola you have an emergency; not because it’s so contagious but because it’s so lethal.”
What the global health community should have learned from previous infectious outbreaks, such as that of HIV, is that responding to them is a case of “act now or pay later”, Piot says. However, it took until July 2014 for the World Health Organisation to convene a high-level emergency meeting – and until August to declare the West African Ebola outbreak a “public health emergency of international concern”.
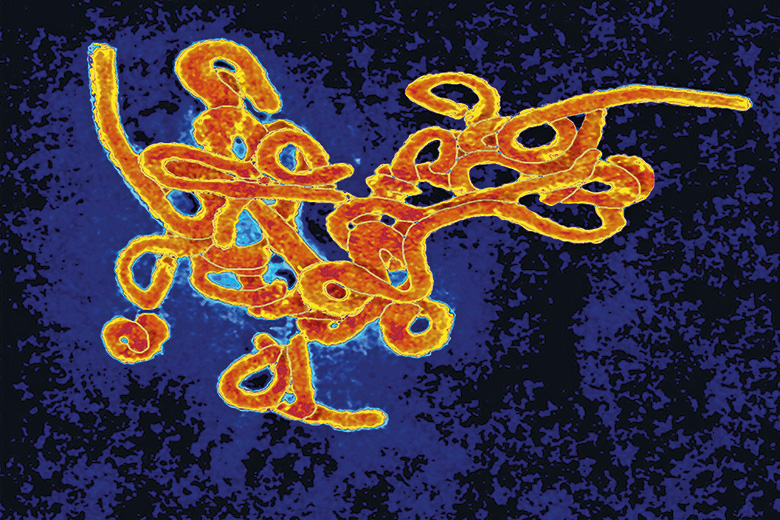
The WHO declaration galvanised governments, funding bodies and universities. The fatality rate for those infected with Ebola was 70 per cent and, without a vaccine or drug, doctors could only maintain hydration, blood pressure and oxygen levels. Potential Ebola vaccines had not been tested in humans and were largely of interest to funders only insofar as they might be used to counter an act of bioterrorism.
“We started saying that something needs to be done,” says Charlie Weller, who leads the Wellcome Trust’s vaccines programme. “And then we moved very quickly once the decision was made to do something; and that something was [addressing the absence of] vaccines or drugs.”
The trust set aside considerable extra funding and put out an emergency call for candidate Ebola vaccines, whose testing and approval could be fast-tracked during the epidemic. The response from the academic community was prompt and energetic.
“Everyone who was involved would work through the night to get the application forms done,” Weller says. “The reviewers would turn around the reviews in days [or even] hours, and the [members of the funding] committee would rearrange their schedules in order to be able to take part in a collective…decision,” Weller says. “It was only because of this that we could move as quickly as we did.”
Meanwhile, at the London School of Hygiene and Tropical Medicine, University of London, Piot threw his support behind staff who wanted to get involved in the relief effort. Recognising that their careers could be affected by their absence, he promised to protect their salaries.
“I’d heard that some American universities had banned their staff from going to West Africa, and [that their staff] needed special permission from the [institution’s] president [to do so],” Piot says. “I said: ‘I’m going to do exactly the opposite.’ I sent [an email] to all staff [saying]: ‘This is a time when we must take up our responsibility; we are a school of public health, of global health: we have a lot of people with a lot of expertise.’” He received 400 responses from a school that only has 1,200 postgraduate students, and 379 academic staff who were eligible for submission to the 2014 research excellence framework. Last year, the school was named University of the Year at the Times Higher Education Awards in recognition of its response to the Ebola crisis.
“I was so pleasantly surprised by the reaction [of our staff to the call],” Piot says. “I was really proud.”

However, Piot’s institution was just one small part of what, by the peak of new Ebola diagnoses in October 2014, had become a massive global response to the emergency. Clinical and military personnel were deployed from all over the world to assist the overwhelmed healthcare systems in the affected countries. Canadian and Chinese mobile laboratories were set up in the region for diagnostic testing, for instance, while Germany sent 400 specially adapted motorbikes for rushing test samples between treatment units and laboratories.
Nor was the response confined to the standard medical disciplines. Virologists and epidemiologists were joined by administrators, social scientists and other researchers who, despite having no background in Ebola, offered their expertise – such as in helping to develop safer burial practices.
For the medics, treating patients with experimental vaccines during an outbreak was unprecedented, but ethics committees had agreed that there was a moral imperative to provide all possible help. And academics hoped that good research, which would benefit their own knowledge and careers, could be carried out at the same time as helping patients, while inconveniencing the exhausted doctors as little as possible.
Without an international body overseeing the response, however, researchers had to scramble for treatment centres and patients. And, faced with conducting clinical trials in sparse facilities with constantly rotating staff and dying patients from whom it was difficult to gain consent, some researchers were forced to strip back their trials to the bare bones. For instance, while conducting a trial for a vaccine candidate called brincidofovir in an MSF treatment centre in Liberia, Trudie Lang, professor of global health research at the University of Oxford, found herself having to boil her trial down to just one key question: is this patient dead or alive?
“We [in the global health research community] run trials in low-resources settings with challenging diseases, in places where research wasn’t really happening before,” says Lang, who is also head of the Global Health Network: an online platform for pooling expertise on global health. “So we’re always trying to find ways of doing trials very efficiently but thoroughly. You focus on asking a very key question and make sure that you measure things that answer that question. You train people really well to focus on the important areas around making sure the patients are safe [and that] everyone’s behaving ethically.”
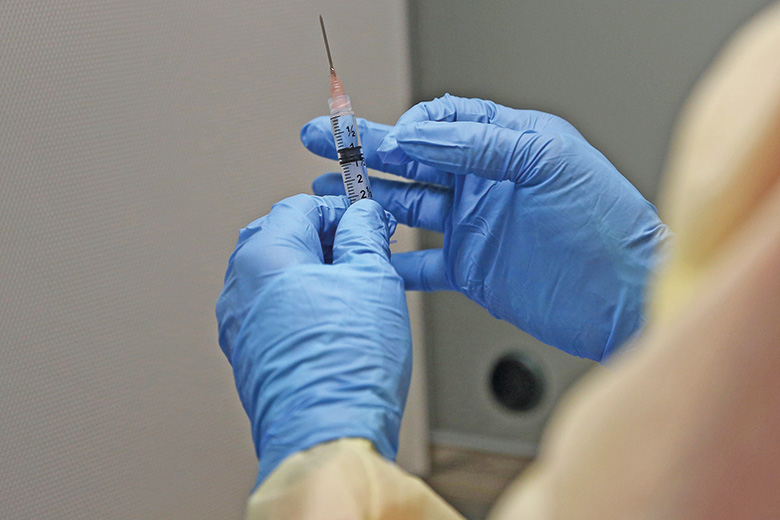
John-Arne Røttingen, director of the division of infectious disease control at the Norwegian Institute of Public Health, headed the phase III trial steering committee for VSV-EBOV, an experimental vaccine donated by the Public Health Agency of Canada for testing during the outbreak. When the trial began in 2015, the number of new Ebola cases in Guinea was falling and the researchers were unable to do a standard randomised controlled trial. Instead, they used a form of the “ring vaccination approach” famously used against smallpox outbreaks in the 1970s. This required tracing all the people who had been in recent contact with an infected patient and vaccinating them, either immediately or after a delay of 21 days. The trial involved 12,000 people in 117 rings.
“In this sort of practice, it’s a trade-off [between] risk and benefit,” Røttingen says. The imperative is to have as short a delay as possible between testing and rolling out the vaccine more widely, consistent with ensuring that the vaccine works. For Røttingen, it was important that people benefited from the research while it was being carried out.

In December 2016, a study was published confirming that VSV-EBOV was safe and offered an effectiveness rate of between 70 and 100 per cent. Yet, by then, the epidemic was already over, having claimed the lives of 11,310 people. Many consider that the number could and should have been much lower.
Researchers describe an array of practical barriers that slowed their pace, including issues with visas, transport, bureaucracy and data and sample sharing between organisations. The committees assembled to review the epidemic response (including a joint panel between Harvard University’s Global Health Institute and the London School of Hygiene and Tropical Medicine, chaired by Piot) concluded that the international community had failed to be – as the UK House of Commons’ Science and Technology Committee described it in its own report – “research ready” for the outbreak.
“We had not taken the promising Ebola [vaccine] candidates from pre-clinical animal studies to human [studies] ahead of the outbreak,” says Røttingen. “If we had done [early] trials ahead of the epidemic – which can be done easily because, of course, you do not need an ongoing transmission – we probably would have been able to start the [phase III] trial half a year earlier at least. And then the vaccine trial itself could have made a huge impact on reducing the number of people getting Ebola.”
One problem, according to Oxford’s Hill, is that there is currently “no business case” for pharmaceutical companies to invest in treatments for diseases such as Ebola. “The average vaccine takes half a billion dollars and decades [to develop], and that’s if it’s straightforward,” he says. There is a strong case, he continues, to reduce dependency on pharmaceutical companies by using philanthropic and public funds for early pre-clinical trials, and to keep vaccination during epidemics affordable by stockpiling those that have been deemed safe but have not yet been commercially licensed. Adopting a new model for vaccine trials could quicken responses to future outbreaks, Hill concludes.
At the 2016 World Economic Forum in Davos, Switzerland, Piot chaired a meeting with representatives from governments, vaccine manufacturers and major funders. He “tested the water” to see whether there was an appetite for a new body to coordinate responses to epidemics, and found that there was.
“There was a need, absolutely, for coordination on the ground,” agrees the Wellcome Trust’s Weller. This is because there needs to be agreement over questions such as how many clinical trials can be done within a certain treatment centre, which treatments are the most promising and which countries and funding bodies should be given priority for their research.
“Different [post-epidemic] panels and reports came to a similar conclusion: that we need a new system to coordinate research and development for health technologies against epidemic threats,” Weller says.
As a result, the Coalition for Epidemic Preparedness Innovations was launched in January at this year’s World Economic Forum. Cepi is intended to be a coalition of public, private and philanthropic bodies aimed at preventing future disease epidemics through rapid vaccine development. With Røttingen as its interim chief executive, it is initially backed by the Wellcome Trust, the Bill and Melinda Gates Foundation and the governments of Norway, Germany and Japan to the tune of nearly $500 million (£402 million).
“This initiative came [from] the experience of all the trials conducted during the Ebola outbreak; there were 16 conducted in less than a year,” says Røttingen. “We managed to condense what takes, on average, eight years from stage one to stage three development [to one year]. That demonstrated the opportunity to do vaccine development for epidemic diseases [much more rapidly].” VSV-EBOV is the only vaccine candidate that has so far been confirmed as effective.
The coalition aims to start phase I and II trials on at least four vaccine candidates against yet-to-be-determined priority pathogens over the next five years, allowing clinical trials to begin in the earliest stages of an outbreak.
For his part, Piot is encouraged by these developments, which he hopes indicate that the global health community will finally stop repeating its past mistakes when it comes to tackling outbreaks of infectious diseases.
He vividly recalls his first visit to the London School of Hygiene and Tropical Medicine in the 1970s, for a meeting organised by the WHO in response to the latest epidemic. “Lessons were [supposedly] learned and promises were made: ‘We will strengthen the infrastructure; we will do this and that,’” he says. “And what happened afterwards? Nothing. We can’t do that a second or a third or a fourth or a fifth time. For me, that is a moral imperative: we owe that to the people who died.”
From the lab to Liberia: ‘Witnessing the devastation strengthened my commitment to vaccine research’
“For me, it was not really a question of if I would go but when,” says Andrea Marzi, a basic virologist who flew out to West Africa during the Ebola epidemic to help in the relief effort. “I’ve been working with the Ebola virus and developing [the VSV-EBOV] vaccine for a long time [but it] was always so abstract.”
Marzi was part of a team that helped develop the ultimately successful vaccine under Heins Feldman, chief of the Laboratory of Virology at the US National Institute of Allergy and Infectious Diseases’ Rocky Mountain Laboratories in Hamilton, Montana. As early as 2005, VSV-EBOV, which consists of a rabies virus engineered to incite an immune response to the Ebola virus, had been shown to be effective in animal studies, and when the West African epidemic erupted, Marzi and her colleagues returned to it.
They carried out studies in macaques and found that the vaccine was effective within seven days. The suggestion was then made that it should be given to the health workers going to the region, but the question remained of how long it would take for those injected with it to build up “a protective level of antibodies, so they could basically go into the field without worrying”.
Marzi twice volunteered to go to West Africa to help with the outbreak response, working at Médecins Sans Frontières’ ELWA 3 treatment unit in Monrovia, Liberia. She first arrived in August 2014: the month in which the WHO declared a “public health emergency” and ELWA 3 was being expanded into the largest Ebola treatment centre ever built.
“In the first few days...we saw quite a few marches of [local] people singing and saying: ‘Ebola is real and you need to protect your family and don’t ignore it; if you have symptoms, go to the treatment unit.’ That was quite astounding.”
During her periods in Liberia, Marzi carried out same-day diagnostic blood tests. Everything was run very precisely, with samples rapidly delivered from the patients to the diagnostics facility and Marzi and her colleagues reporting back to the doctors after just a few hours about whether the patients were infected.
For Marzi, seeing “how much tragedy and devastation an outbreak can cause strengthened my belief...that I really want to continue this vaccine research”, she says. “I always loved what I did but when I saw its impact on the ground, I thought to myself: ‘Yes, I should definitely keep doing this!’”
Hilary Lamb
Treatment centres: ‘We were conducting clinical research in a tent’

“I think this really was more than an outbreak,” says Peter Horby, professor of emerging infectious diseases and global health at the University of Oxford.
“There are always outbreaks, [but] this was turning into a humanitarian crisis: three countries affected and predictions of potentially millions of cases; whole countries basically shut down.”
When the Wellcome Trust put out its emergency calls for vaccine candidates, Horby pulled together collaborators to work on trials for two candidates: brincidofovir – which was shut down quickly – and TKM. He flew to West Africa, where Médecins Sans Frontières had arranged a tour of its treatment centres. However, because of the variation between centres, the constant rotation of volunteers and the deaths of patients, finding the right location was a challenge.
“We [travelled] across three countries,” Horby says. “The first we visited, in Conakry in Guinea, was starting to crumble. The other extreme was a brand new facility being purpose-built in Sierra Leone. We went to centres that were in crisis, trying to manage patients [and, at the other extreme, to] centres where most of the staff were twiddling their thumbs because most of the crisis had passed.”
Each morning, Horby and his colleagues met the clinical teams running the centres to see if there were any new patients that met the criteria for inclusion in the trial. If there were, Horby’s team would put on protective equipment to enter the facility and explain the trials to the quarantined patients to see if they were willing to be enrolled.
“It’s difficult to gain consent when you’re wearing an Ebola suit and the patients can’t see you and hear you properly,” Horby says. “Sometimes patients are too unwell to give consent.”
The team had to run to a very tight rota as there was only a certain amount of time that an individual could remain in the scorching treatment centre wearing protective equipment. It was almost like a military operation, Horby says. But it was still extremely difficult and, despite the suits, a foreign healthcare worker became infected with Ebola on the first day of the trial, resulting in the need to quarantine half the research staff.
“We were conducting clinical research – intravenous infusions of highly experimental drugs – in a tent with intermittent electricity,” Horby points out. “But it was an amazing experience to have that kind of commitment from people: [to see] the willingness of people to dedicate their time and [risk] their own personal safety to get this done. It was extremely invigorating.”
Hilary Lamb
Containment and cure: science in action

In the battle to maintain or increase higher education and research’s share of the public funding pie, we have to show that our work makes a difference. Publishing papers in highly cited, big name journals is important, but basically meaningless to anyone outside academia.
Even the impact case studies generated for the UK’s research excellence framework are unlikely to be read by many people outside policy circles. But, as the sector’s response to the Ebola crisis clearly demonstrates, overseas aid is one area where our work has an impact so important that it grabs headlines in the national as well as the academic press.
Scientists are an essential part of any effective overseas aid effort. Anyone can buy a bag of rice for the victims of the latest pandemic: not so many people can set up a high-level bio-containment lab with an intermittent power supply. And doing science relevant to emerging infections wins on multiple levels. It benefits the countries where the pathogens are occurring and protects the countries to which they might spread. It benefits the science community, answering specific questions, training researchers and building networks. But it also works politically.
In the UK, the sizeable official development assistance spend – required in law to amount to 0.7 per cent of gross domestic product – is not universally popular. Spending some of the money allotted for aid on UK science keeps the money in the country, supporting highly skilled jobs and infrastructure, while also addressing global problems. And it is already happening. Examples include the £735 million Newton Fund , aimed at developing science partnerships with the developing world “that promote the economic development and welfare of collaborating countries”, and the £1 billion Ross Fund to help combat serious infectious diseases in developing countries by developing new vaccines, drugs and diagnostics. The recent launch of the Coalition for Epidemic Preparedness Innovations is a more international example.
But for targeted pandemic research to be effective, you need to be able to predict which pathogens will flip into global threats. While Ebola had been on the global health agenda for some time, few would have predicted the emergence of Zika or Middle East Respiratory Syndrome (Mers). For any given rapidly emerging pandemic infection, the research effort is behind the curve, and although there are approaches being set in place to mitigate these problems, a sole focus on translational research is not the only answer.
Investing in basic science is also important. We need a corps of scientists trained in broad, basic methods that can be applied flexibly to a range of scenarios. An example is the UK Public Health Rapid Support Team : a £20 million government-funded scheme established in the wake of the Ebola crisis to maintain a specialist team that can be deployed anywhere in the world within 48 hours to tackle disease outbreaks with the potential to develop into pandemics.
Basic research improves lives. From epidemiological modellers and vaccine trial units in the UK, to clinical researchers and lab virologists working in the field, we should celebrate and shout from the rooftops the role higher education played in treating, containing and eradicating Ebola in West Africa.
John Tregoning is senior lecturer in the mucosal infection and immunity section of virology at Imperial College London.
POSTSCRIPT:
Print headline: Healing hands
Register to continue
Why register?
- Registration is free and only takes a moment
- Once registered, you can read 3 articles a month
- Sign up for our newsletter
Subscribe
Or subscribe for unlimited access to:
- Unlimited access to news, views, insights & reviews
- Digital editions
- Digital access to THE’s university and college rankings analysis
Already registered or a current subscriber? Login