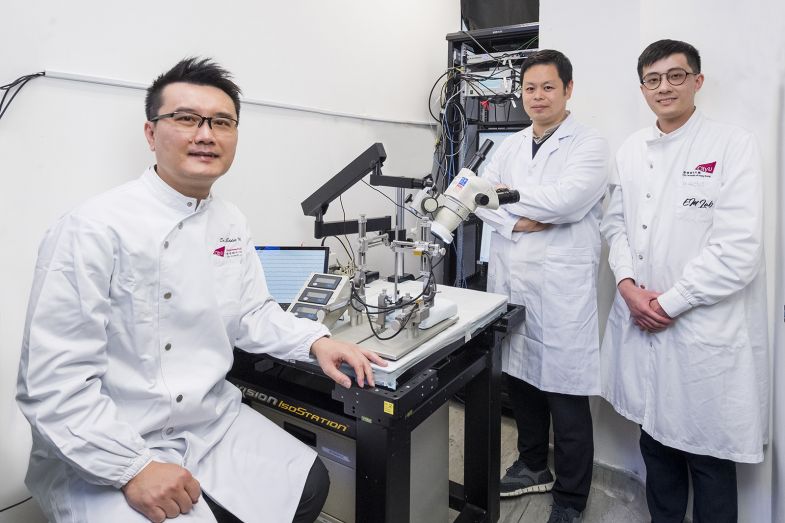
(From left) Dr Eddie Ma Chi-him, Dr Vincent Ko Chi-chiu and Dr Au Ngan-pan
A small molecule identified by CityU researchers for the first time offers hope for patients with optic nerve damage such as glaucoma-related vision loss.
Named M1, the molecule can restore the visual function in the mammalian central nervous system (CNS).
It works by stimulating the fusion and motility of mitochondria (the powerhouse of a cell to generate energy) and induces robust axon regeneration by enhancing the intrinsic growth capacity of injured neurons.
This is excellent news because traumatic injuries to the CNS, including the optic nerve, the brain and the spinal cord, are the leading causes of disability worldwide for which there is no available treatment.
Led by Professor Eddie Ma Chi-him, Associate Head and Associate Professor in the Department of Neuroscience and Director of the Laboratory Animal Research Unit at CityU, this research breakthrough heralds a new approach that could address unmet medical needs in accelerating functional recovery within a limited therapeutic time window after CNS injuries.
“Photoreceptors in the eyes [retina] forward visual information to neurons in the retina. To facilitate the recovery of visual function after injury, axons of neurons must regenerate through the optic nerve and relay nerve impulses to visual targets in the brain via the optic nerve for image processing and formation,” said Professor Ma.
M1 treatment sustains long-distance axon regeneration from the optic chiasm, i.e.,
midway between the eyes and target brain region, to multiple subcortical visual targets in the brain.
“Regenerated axons elicit neural activities in target brain regions and restore visual functions after M1 treatment. Our study highlights the potential of a readily available and non-viral therapy for CNS repair,” he added.
The seven-year-long study builds on the team’s previous research on peripheral nerve regeneration using gene therapy.
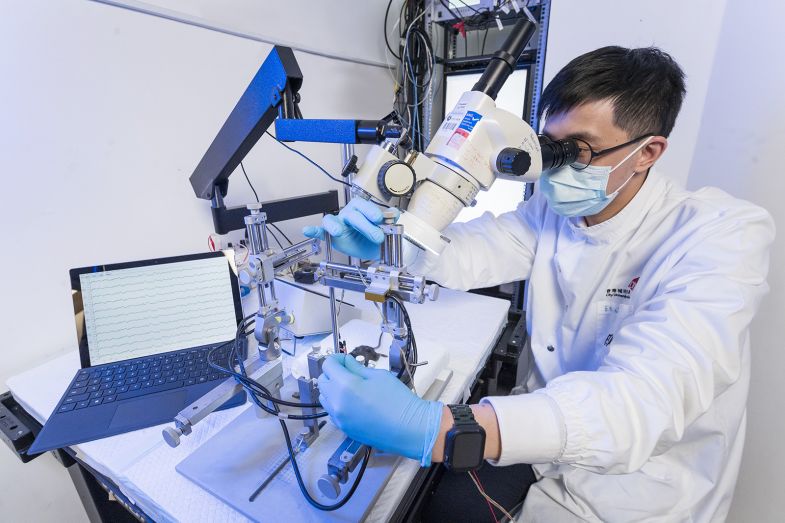
Regenerated axons elicit neural activities in target brain regions and restore visual functions after M1 treatment. The computer screen at the left side of the photo indicates such brain activities
“This time we have used the small molecule M1 for repairing CNS simply by intravitreal injection into the eyes, which is an established medical procedure for patients, i.e., for macular degeneration treatment.
Successful restoration of the visual function such as pupillary light reflex and responses to looming visual stimuli, e.g., visually induced innate defensive responses to avoid predators, was observed only in M1-treated mice four to six weeks after the optic nerve had been damaged, said Dr Au Ngan-pan, Research Associate in the Department of Neuroscience.
The research team is developing an animal model for treating glaucoma-related vision loss using M1 and possibly other common eye diseases and vision impairments such as diabetes-related retinopathy, macular degeneration and traumatic optic neuropathy. Thus further investigation is warranted to evaluate the potential clinical application of M1.
“Nerve regeneration and function recovery will help improve the quality of life for patients and reduce the burden on the local community and healthcare systems,” Dr Ma added.